
CATEGORY 1 CME
Premiere Date: June 20, 2025
Expiration Date: December 20, 2026
This exercise affords CE credit for:
1. Physicians (CME)
2. Different
All different clinicians both will obtain a CME Attendance Certificates or might select any of the sorts of CE credit score being provided.
ACTIVITY GOAL
To know the epidemiology of Parkinson illness signs.
LEARNING OBJECTIVES
1. Focus on the epidemiology of neuropsychiatric signs of Parkinson illness.
2. Describe the evaluation of neuropsychiatric signs of Parkinson illness.
3. Enumerate the evidence-based therapies for neuropsychiatric signs of Parkinson illness.
TARGET AUDIENCE
This accredited persevering with training (CE) exercise is meant for psychiatrists, psychologists, main care physicians, doctor assistants, nurse practitioners, and different well being care professionals who search to enhance their take care of sufferers with psychological well being issues.
ACCREDITATION/CREDIT DESIGNATION/FINANCIAL SUPPORT
This exercise has been deliberate and carried out in accordance with the accreditation necessities and insurance policies of the Accreditation Council for Persevering with Medical Training (ACCME) by way of the joint providership of Physicians’ Training Useful resource,® LLC and Psychiatric Instances®. Physicians’ Training Useful resource, LLC, is accredited by the ACCME to supply persevering with medical training for physicians.
Physicians’ Training Useful resource, LLC, designates this enduring materials for a most of 1.5 AMA PRA Class 1 Credit.™ Physicians ought to declare solely the credit score commensurate with the extent of their participation within the exercise.
This exercise is funded totally by Physicians’ Training Useful resource, LLC. No industrial assist was acquired.
OFF-LABEL DISCLOSURE/DISCLAIMER
This accredited CE exercise might or might not focus on investigational, unapproved, or off-label use of medication. Contributors are suggested to seek the advice of prescribing data for any merchandise mentioned. The knowledge supplied on this accredited CE exercise is for persevering with medical training functions solely and isn’t meant to substitute for the impartial scientific judgment of a doctor relative to diagnostic or therapy choices for a selected affected person’s medical situation. The opinions expressed within the content material are solely these of the person school members and don’t mirror these of Physicians’ Training Useful resource, LLC.
FACULTY, STAFF, AND PLANNERS’ DISCLOSURES AND CONFLICT OF INTEREST MITIGATION
Not one of the workers of Physicians’ Training Useful resource, LLC, or Psychiatric Instances or the planners or the authors of this academic exercise have related monetary relationship(s) to reveal with ineligible firms whose main enterprise is producing, advertising, promoting, reselling, or distributing well being care merchandise utilized by or on sufferers.
For content-related questions, electronic mail us at PTEditor@mmhgroup.com; for questions regarding the accreditation of this CME exercise or the way to declare credit score, please contact information@gotoper.com and embrace “Impulse Management Issues, Psychosis, and Cognitive Impairment in Parkinson Illness” within the topic line.
HOW TO CLAIM CREDIT
After getting learn the article, please use the next URL to judge and request credit score: https://training.gotoper.com/exercise/ptcme25june. If you don’t have already got an account with Physicians’ Training Useful resource, LLC, you’ll be prompted to create one. You need to have an account to judge and request credit score for this exercise.
Editor’s Be aware: Please see the April CME article for extra data on despair, apathy, and nervousness in Parkinson illness.
Neuropsychiatric signs (NPS) are widespread amongst people with Parkinson illness (PD), with cross-sectional research indicating prevalence charges of 70% to 89%.1 Though widespread, these signs are sometimes underrecognized and never adequately handled, including to the incapacity brought on by the sickness.2 NPS which can be seen amongst people with PD embrace despair, apathy, nervousness, impulse management issues (ICDs), psychosis, and cognitive impairment together with dementia. Melancholy, apathy, and nervousness have been coated in Half 1 of this CME exercise.
Psychosis
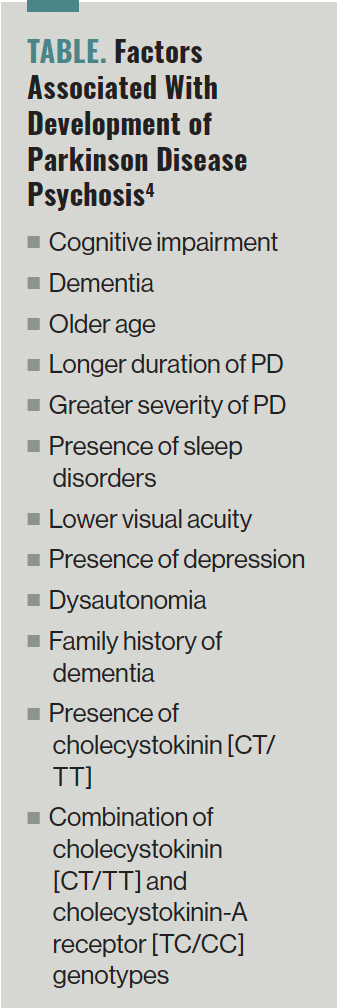
A meta-analysis by Chendo et al discovered that amongst people with PD, the pooled frequency of psychosis (hallucinations, delusions, and minor psychotic phenomena, together with sense of presence, passage hallucinations, and illusions) was 20.7%.3 In one other research, the investigators famous that visible hallucinations have been current in roughly 1 / 4 to a 3rd of people with PD and auditory hallucinations have been seen in about 20% of the people. Minor phenomena have been seen in roughly 17% to 72% of the people and delusions have been famous amongst 5% of the folks with PD.4 In keeping with information, additional components related to the event of PD psychosis (PDP) may be discovered within the Desk.4
TABLE. Elements Related With Improvement of Parkinson Illness Psychosis4
Outcomes of 1 research confirmed that amongst people with PD and hallucinations at baseline (33%), the incidence of the hallucinations elevated to 44% at 18 months and 63% at 48 months (P <.0001).5 The investigators discovered that point was the one important issue influencing the event of hallucinations over the 48-month interval. In lots of of those circumstances, hallucinations might develop into worse. One research discovered that hallucinations worsened in 95% of circumstances throughout a 3-year follow-up interval. A latest meta-analysis additionally discovered a big constructive affiliation between psychosis and cognitive impairment (standardized imply distinction [SMD], 0.44), and psychosis and illness development (SMD, 0.46).6
Outcomes of one other meta-analysis confirmed that people with PDP have worse performing on all main cognitive domains when put next with people with PD, however with out psychosis together with international cognition (Hedges g = —0.57), processing velocity (Hedges g = —0.58), government capabilities (Hedges g = —0.56), episodic reminiscence (Hedges g = —0.58), and notion (Hedges g= —0.55) because the almost certainly affected domains.7 One other meta-analysis discovered that people with PDP had decrease gray matter quantity (GMV) in parietal-temporo-occipital areas and the GMV loss in PDP was related to native gene expression of 5-HT1a (P = .012) and 5-HT2a receptors (P = .002) however not dopaminergic receptors.8
The consensus tips developed by the Nationwide Institute of Neurological Issues and Stroke and the Nationwide Institute of Psychological Well being working group for the prognosis of PDP point out that for making a prognosis of PDP, a confirmed prognosis of PD with the onset of 1 or extra PDP-associated signs together with hallucinations, illusions, delusions, or false sense of presence with a period of not less than 1 month ought to be current.9 Additionally it is essential to rule out secondary causes of psychosis together with medical, psychiatric, medicine results, and substance use issues. A prognosis of PDP may be made if the psychotic signs proceed regardless of elimination of different potential causes for psychosis.10 Half 1 of the Motion Dysfunction Society Unified Parkinson’s Illness Score Scale (UPDRS) and the improved Scale for the Evaluation of Optimistic Signs in PD which can be accomplished with the sufferers and their caregivers can help within the prognosis of PDP.
One meta-analysis discovered that cholinesterase inhibitors (CHIs) improved delusions (SMD, −0.14; P = .04) and hallucinations (SMD, —0.08; P = .01) amongst people with PD.11 Though there have been no important variations famous among the many varied CHIs, rivastigmine confirmed the biggest impact dimension for each delusions (SMD, —0.11; P = .03) and hallucinations (SMD, —0.10; P = .01). The investigators additionally discovered a big impact dimension for CHIs on the full neuropsychiatric rating (SMD, —0.18; P = .002). Additionally they famous a big interplay between the therapy impact and the baseline neuropsychiatric whole rating (P = .02) when put next with placebo, indicating that a rise in baseline neuropsychiatric rating elevated the impact dimension in favor of medicine therapy. A major interplay between therapy end result of whole neuropsychiatric rating and baseline Mini Psychological State Examination (MMSE) rating was famous (P = .008), indicating {that a} lower in baseline MMSE rating elevated the impact dimension in favor of medicine therapy when put next with placebo.
In one other community meta-analysis, Yunusa et al discovered that on the Medical World Impression Scale for Severity, pimavanserin (SMD, —4.81), clozapine (SMD, —4.25), and quetiapine (SMD, —1.15) considerably improved severity of psychotic signs when put next with placebo.12 On the Scale for Evaluation of Optimistic Signs for Parkinson Illness, pimavanserin (OR, 1.16) improved psychotic signs when put next with placebo. On the UPDRS, clozapine (SMD, −0.69), pimavanserin (SMD, —0.01), and quetiapine (SMD, 0.00) didn’t impair motor functioning. Quetiapine (SMD, 0.60) impaired cognition (MMSE scores) when put next with placebo. Outcomes of this research discovered that pimavanserin and clozapine have been most efficacious and protected with pimavanserin having the best likelihood of being efficacious when used amongst people with PDP. Pimavanserin is FDA authorized for the therapy of PDP.
In a second community meta-analysis, Srisurapanont et al discovered that clozapine (SMD, —1.31) and pimavanserin (SMD, —0.30) have been superior to the placebo in treating psychotic signs amongst people with PD, whereas quetiapine (SMD, 0.47) was discovered to be inferior to placebo.13 Clozapine was ranked first in decreasing psychotic signs (P-score = 1.00), adopted by pimavanserin (P-score = 0.73). Clozapine was ranked first (P-score = 0.81) in stopping the worsening of irregular actions. The authors concluded that clozapine emerged because the medicine with the best efficacy (giant therapy impact) and exhibited minimal motor adversarial results, had excessive acceptability and average general tolerability. Pimavanserin was ranked second by way of efficacy (small-to-moderate therapy impact) and was related to average motor adversarial results, general tolerability, and acceptability.
One meta-analysis that evaluated information from 5 research discovered that electroconvulsive remedy (ECT) was efficient in treating psychotic signs amongst people with PD (SMD, 1.64, P <.001).14 Outcomes of this research additionally confirmed that cognition improved after ECT amongst these people (SMD, 0.21; P = .002).
Out there proof from these research signifies that pimavanserin and clozapine are first-line medicines to deal with psychotic signs amongst people with PD. Quetiapine may be thought of as a second-line medicine to deal with signs of PDP. CHIs, particularly rivastigmine, may be helpful in therapy of PDP. ECT can be utilized for the therapy of psychotic signs that aren’t amenable to therapy with pimavanserin, clozapine, and/or quetiapine.
ICDs
ICDs are characterised by an incapability to withstand an inappropriate drive, leading to repetitive behaviors that may result in dangerous penalties to the person.15 The commonest ICDs embrace pathological playing, compulsive sexual conduct, compulsive consuming, and compulsive purchasing. ICDs are seen in roughly 18.5% of people with PD.16 Impulsive-compulsive behaviors (ICBs) discuss with repetitive, extreme, and compulsive behaviors which can be pushed by some robust need and are sometimes tough to manage. ICBs are seen in roughly 14.64% of people with PD.17
Out there proof signifies that the ICD worsens high quality of life, actions of day by day dwelling, and emotional well-being (P <.004) amongst people with PD.18 One meta-analysis discovered that when put next with people who’ve PD and no ICD, people with PD and ICD had worse abstraction means/idea formation (Hedges g = —0.40), set shifting (Hedges g = —0.59 and —0.46), visuospatial/constructional means (Hedges g = —0.42), and decision-making (Hedges g = 0.54).19
One meta-analysis that included information from 15 research discovered that threat components for people with PD growing ICD have been youthful age (SMD, —0.39, P <.01), male intercourse (OR, 1.64; P <.01), smoking behavior (OR, 2.28; P = .02), dopamine receptor agonist (DA) use (OR, 3.41; P <.01), DA equal day by day dose (SMD, 0.42; P = .003), levodopa equal day by day dose (whole LEDD; SMD, 0.32; P <.01), and amantadine use (OR, 2.26; P <.01).20
ICBs have been famous to be extra widespread amongst Caucasians (17.9%) than amongst Asians (12.4%) with PD.17 Danger components for ICBs amongst people with PD are youthful age (P <.0001), male intercourse (OR, 1.64; P = .001), longer course of PD (P = .005), greater despair scores (Hamilton Melancholy Score Scale, P = .007), extra levodopa dosage (P = .02), DA use (P <.00001), greater common dose (levodopa, P = .0003; DA, P <.00001), in addition to extra amantadine use (P = .0004). One meta-analysis additionally discovered that speedy eye motion conduct dysfunction was related to a greater than 2-fold higher threat of growing ICBs (OR, 2.12; P <.01).21
A meta-analysis discovered that there have been no important adjustments in any cortical or subcortical areas amongst people with PD and ICD.22 Nevertheless, there was elevated exercise famous within the ventral striatum and orbitofrontal cortex and decreased exercise in anterior cingulate cortex (ACC) amongst these people. Moreover, clusters of hyperactivation in ventral striatum and of hypoactivation in ACC have been additionally famous within the meta-analysis. These findings point out strongly that ICD in PD is expounded to a dysfunction of limbic divisions of the striatum and of the prefrontal cortex. One meta-analysis discovered that there was no important impairment recognized in reward processing in sufferers with PD and ICD when put next with sufferers with PD and with out ICD (SMD, −0.02; 95% CI, —0.43-0.39).
A prognosis of ICD is made by way of a scientific interview with the person with PD and their caregivers.23 Questionnaire for ICDs in PD and Questionnaire for ICDs in PD Score Scale are validated scales with a sensitivity of 96% and 94%, respectively, in figuring out ICDs amongst people with PD.24
Though there aren’t any meta-analyses which have evaluated the therapies for ICDs amongst people with PD, therapy suggestions embrace decreasing and even withdrawing DAs as a first-line technique.25 Using intrajejunal levodopa that gives steady drug supply to the physique or utilizing amantadine, which acts as a dopaminergic and glutamatergic modulator, might profit some people with ICD with out aggravating motor capabilities. Restricted information additionally point out some profit from valproate, zonisamide, naloxone, apomorphine, and bromocriptine amongst people with ICD. Clozapine could also be helpful for the therapy of refractory ICDs amongst people with PD.26 Though the info are restricted, a couple of research additionally advocate subthalamic nucleus deep mind stimulation as a therapy for ICDs.25 Low-frequency repetitive transcranial magnetic stimulation (rTMS) over the dorsolateral prefrontal cortex has additionally been famous to be helpful amongst people with PD and ICBs.27 One randomized managed trial that in contrast as much as 12 classes of a cognitive conduct remedy (CBT)-based intervention to a ready listing management situation with commonplace medical care indicated that ICBs improved considerably within the therapy group when put next with controls (P = .03).28
These research point out that discontinuation of DAs and the usage of CBT could also be first choices for treating ICDs/ICBs amongst people with PD. Drugs resembling clozapine and coverings resembling rTMS could also be helpful amongst refractory circumstances of ICDs/ICBs.
Cognitive Impairment
Amongst people with PD, cognitive impairment is likely one of the main nonmotor signs.29 Cognitive impairment presents insidiously amongst people with PD and contains impairments in planning, working reminiscence, government dysfunction, consideration, semantic verbal fluency, and visible spatial means. People with PD might subsequently develop gentle cognitive impairment (MCI), which can progress to dementia. Outcomes of a meta-analysis discovered that postural-instability-gait dysfunction (RR, 3.76), hallucinations (RR, 3.09), orthostatic hypotension (RR, 2.98), cerebrovascular illness (RR, 1.52), diabetes (RR, 1.47), weight problems (RR, 1.38), cardiac illness (RR, 1.35), and alcohol consumption (RR, 1.32) improve the danger for cognitive impairment amongst people with PD.30
One meta-analysis discovered that the pooled prevalence of MCI was 40%, with the next frequency for the a number of area subtype (31%) of MCI to be seen amongst people with PD.31 Danger components for growing MCI in PD have been older age (Hedges g = 0.36), male intercourse (Hedges g = 0.10), decrease ranges of training (Hedges g = —0.29), an extended illness period (Hedges g = 0.18), use of upper LEDD (Hedges g = 0.25), greater Hoehn and Yahr stage (Hedges g = 0.33), greater UPDRS motor scores (Hedges g = 0.40), postural instability/gait problem motor subtype vs tremor dominant subtype (46% vs 35%; P <.001), despair (Hedges g = 0.29), apathy (Hedges g = 0.41), and a poorer high quality of life (Hedges g = 0.18). One meta-analysis that included information from 39 research discovered that inside 3 years, 25% of people with PD and regular cognition transformed to PD-MCI, and a pair of% transformed to dementia.32 Of these with PD-MCI, 20% transformed to dementia, whereas 28% reverted to a state of regular cognitive operate. The investigators famous that the conversion charges to MCI and dementia have been greater and reversion charges have been decrease when the follow-up was equal to or longer than 3 years. A meta-analysis revealed that amongst all of the cognitive domains (Hedges g = 0.47), measures of government functioning (Hedges g = 0.70) predicted the conversion of people with PD-MCI to PD dementia (PDD).33
One meta-analysis discovered that the worldwide pooled dementia frequency amongst people with PD was 26.3%.34 The pooled frequency of dementia was higher amongst people aged 75 years or older (43.4%), lower than or equal to 4 years of training (29.2%), 15 years or longer of PD period (40.9%), and higher than 3 on the Hoehn and Yahr stage (45.9%). A latest meta-analysis discovered that the pooled incidence charge of PDD was 4.45 per 100 person-years in danger, equating to a 4.5% annual threat of dementia in a PD-prevalent inhabitants.35 The relative threat of PDD was estimated to be 3.25 occasions higher than in wholesome controls. One other meta-analysis discovered that the event of PDD was positively related to older age (OR, 1.07), male intercourse (OR, 1.33), greater UPDRS half III scores (RR, 1.04), presence of hallucinations (OR, 2.47), REM sleep conduct dysfunction (OR, 8.38), smoking (ever vs by no means: RR, 1.93), and hypertension (OR, 1.57).36 An inverse affiliation was discovered between training (RR, 0.94) and the event of PDD. One meta-analysis that included information from 17 research analyzed the affect of the APOE gene on PDD onset from 3 facets: 5 genotypes vs ε3/3, ε2+/ε4+ vs ε3/3, and ε4+ vs ε4−, and located that the danger components for PDD embrace the genotypes ε3/4 (OR, 1.47) and ε4/4 (OR, 2.93; 95% CI, 1.20-7.14).37 The danger of PDD was 1.61 occasions higher in ε4+ people when put next with ε3/3 people (OR, 1.61; P = .0003). Amongst people with PD, the dementia threat of these with ε4+ was 1.72 occasions higher than that of these with ε4− (OR, 1.72; P <.00001).
It is very important recurrently consider cognitive functioning amongst people with PD given the prevalence of cognitive impairment amongst them.38 The presence of a cognitive dysfunction may be recognized utilizing validated screening instruments or by way of a proper neuropsychological evaluation. Additionally it is essential to finish a full medical examination together with laboratory workup to rule out the potential medical causes for cognitive impairment. The Worldwide Parkinson and Motion Dysfunction Society recommends 3 score scales primarily based on their clinimetric properties to measure international cognitive efficiency amongst people with PD.39 These 3 scales are the Montreal Cognitive Evaluation (MoCA), the Mattis Dementia Score Scale Second Version, and the Parkinson’s Illness-Cognitive Score Scale. The MoCA is probably the most steadily used cognitive screening software in scientific follow and analysis research amongst people with PD. Out there proof signifies that normed neuropsychological checks throughout a number of cognitive domains can constantly detect cognitive deficits amongst people with PD, however relative PD efficiency is considerably affected by the inclusion and the kind of wholesome controls vs the usage of revealed norms solely.40 It can be crucial that the number of checks be accomplished primarily based on the presence of ample native inhabitants norms.
At present, there aren’t any FDA-approved nonpharmacologic or pharmacologic therapies for MCI amongst people with PD.41 Preliminary proof signifies that cognitive coaching and bodily train might have short-term advantages on government functioning amongst people with PD.38 Multidomain computer-based cognitive coaching at a frequency of two or 3 occasions per week over 3 to 12 weeks might enhance government capabilities, reminiscence, processing velocity, and a spotlight.38 Cardio train, resistance train, and mixed bodily and cognitive coaching might present short-term advantages on international cognition, processing velocity, sustained consideration, psychological flexibility, and reminiscence amongst people with PD.38
Simply oral rivastigmine is FDA authorized for the therapy of mild-to-moderate PDD.38 One meta-analysis discovered that amongst people with PDD, when put next with placebo, CHI therapy improved scores on the Alzheimer Illness Cooperative Research—Medical World Impression of Change (P <.0001).42 For cognitive operate, a pooled estimate of the impact of CHIs on measures of cognitive operate confirmed therapeutic profit (SMD, —0.34; P <.00001). There was additionally a constructive impact of CHIs on the MMSE (weighted imply distinction [WMD], 1.09; P = .0008). For actions of day by day dwelling, mixed information for the Alzheimer Illness Cooperative Research—Medical World Impression of Change and the UPDRS score scales favored therapy with CHIs (SMD, —0.20; P = .03). For security and tolerability, these taking a CHI have been extra more likely to expertise an adversarial occasion (OR, 1.64; P = .0003) and to drop out (OR, 1.94; P = .0006). Adversarial occasions have been extra widespread amongst these taking rivastigmine (OR, 2.28; P <.0001) however not these taking donepezil (OR, 1.24; P = .25). Tremors (OR, 2.71; P = .002), however not falls (P = .39), have been extra widespread within the therapy group nevertheless it didn’t have a big influence on the UPDRS (whole and motor scores, P = .71). Fewer deaths occurred within the therapy group than within the placebo group (OR, 0.28; P = .03).
One other meta-analysis that included information from 10 trials discovered that CHIs and memantine produced small international results on clinicians’ international impression of change (WMD, —0.40 to WMD, —0.65).43 Nevertheless, simply CHIs and never memantine improved cognition on the MMSE (WMD, 1.04 to 2.57 vs 0.45). Rivastigmine confirmed an elevated threat of adversarial occasions when put next with placebo (RR, 1.19), though these have been gentle or average, and the danger disappeared on critical adversarial occasions.
A 3rd meta-analysis research that solely included individuals with PD discovered that CHIs considerably slowed MMSE decline (MD, —1.123; P = .0010) with none impact on threat of falls (OR, 1.134; P = .681).44 The charges of tremors (OR, 2.805; P = .001) and adversarial drug reactions (OR, 1.86; P <.0001) have been considerably elevated in sufferers receiving CHIs in contrast with placebo. In comparison with placebo, the Alzheimer’s Illness Evaluation Scale–Cognitive Subscale (SMD, —0.266; P <.0001), international evaluation (SMD, —0.287, P <.0001), and behavioral disturbances (SMD, —0.152; P = .025) improved within the CHI group with none impact on incapacity (SMD, —0.134; P = .053). There have been no important variations between the two teams on the UPDRS half III scores (SMD, 0.054; P = .805). The loss of life charge was lowered within the CHI group when put next with placebo (OR, 0.295; P = .017).
In a fourth meta-analysis, investigators decided that people with PDD who acquired donepezil (SMD, 0.51; P <.00001) or rivastigmine (SMD, 0.45; P <.00001) discovered advantages on international cognitive scores when put next with placebo.45 On the Medical World Impressions of Change scale, important enhancements have been famous in individuals who acquired rivastigmine when put next with placebo (RR, 1.37). Rivastigmine in PDD supplied a big profit for tremor when put next with placebo (MD, —2.32; P <.00001). Simply people handled with rivastigmine skilled considerably extra adversarial occasions when put next with placebo (RR, 1.18; P = .0001).
These research point out that nonpharmacologic therapies resembling cognitive coaching and bodily train might have short-term advantages on cognition amongst people with PD. Oral rivastigmine is the one FDA-approved agent for the therapy of mild-to-moderate PDD, though different CHIs could also be of profit amongst people with PDD.
Concluding Ideas
NPS are seen generally amongst people with PD. These embrace despair, apathy, nervousness, ICDs, psychosis, and cognitive impairment together with dementia. Regardless of being widespread, the NPS are poorly recognized and poorly handled amongst people with PD. NPS worsen morbidity and high quality of life amongst people with PD. Out there proof signifies advantages for nonpharmacologic therapies, pharmacotherapeutic brokers, and for mind stimulation strategies amongst people with PD who’ve NPS. Earlier identification and applicable therapy of people with PD who’ve NPS will considerably enhance the lives of those people and people of their caregivers.
Dr Tampi is professor and chairman of the Division of Psychiatry at Creighton College Faculty of Drugs and Catholic Well being Initiatives Well being Behavioral Well being Companies in Omaha, Nebraska. He’s additionally an adjunct professor of psychiatry at Yale Faculty of Drugs, New Haven, Connecticut. Ms Snyder is a medical pupil at Creighton College Faculty of Drugs, Omaha, NE.
References
1. Dlay JK, Duncan GW, Khoo TK, et al. Development of neuropsychiatric signs over time in an incident Parkinson’s illness cohort (ICICLE-PD). Mind Sci. 2020;10(2):78.
2. Jones S, Torsney KM, Scourfield L, et al. Neuropsychiatric signs in Parkinson’s illness: aetiology, prognosis and therapy. BJPsych Advances. 2020;26(6):333-342.
3. Chendo I, Silva C, Duarte GS, et al. Frequency and traits of psychosis in Parkinson’s illness: a scientific evaluation and meta-analysis. J Parkinsons Dis. 2022;12(1):85-94.
4. Fénelon G, Alves G. Epidemiology of psychosis in Parkinson’s illness. J Neurol Sci. 2010;289(1-2):12-17.
5. Goetz CG, Leurgans S, Pappert EJ, et al. Potential longitudinal evaluation of hallucinations in Parkinson’s illness. Neurology. 2001;57(11):2078-2082.
6. Burchill E, Watson CJ, Fanshawe JB, et al. The influence of psychiatric comorbidity on Parkinson’s illness outcomes: a scientific evaluation and meta-analysis. Lancet Reg Well being Eur. 2024;39:100870.
7. Pisani S, Gosse L, Wieretilo R, et al. Cognitive and government impairments in Parkinson’s illness psychosis: a Bayesian meta-analysis. J Neurol Neurosurg Psychiatry. 2024;95(3):277-287.
8. Pisani S, Gunasekera B, Lu Y, et al. Gray matter quantity loss in Parkinson’s illness psychosis and its relationship with serotonergic gene expression: a meta-analysis. Neurosci Biobehav Rev. 2023;147:105081.
9. Ravina B, Marder Okay, Fernandez HH, et al. Diagnostic standards for psychosis in Parkinson’s illness: report of an NINDS, NIMH work group. Mov Disord. 2007;22(8):1061-1068.
10. Pagan FL, Schulz PE, Torres-Yaghi Y, Pontone GM. On the optimum prognosis and the evolving function of pimavanserin in Parkinson’s illness psychosis. CNS Medicine. 2024;38(5):333-347.
11. d’Angremont E, Begemann MJH, van Laar T, Sommer IEC. Cholinesterase inhibitors for therapy of psychotic signs in Alzheimer illness and Parkinson illness: a meta-analysis. JAMA Neurol. 2023;80(8):813-823.
12. Yunusa I, Rashid N, Seyedin R, et al. Comparative efficacy, security, and acceptability of pimavanserin and different atypical antipsychotics for Parkinson’s illness psychosis: systematic evaluation and community meta-analysis. J Geriatr Psychiatry Neurol. 2023;36(5):417-432.
13. Srisurapanont M, Suradom C, Suttajit S, et al. Second-generation antipsychotics for Parkinson’s illness psychosis: a scientific evaluation and community meta-analysis. Gen Hosp Psychiatry. 2024;87:124-133.
14. Takamiya A, Seki M, Kudo S, et al. Electroconvulsive remedy for Parkinson’s illness: a scientific evaluation and meta-analysis. Mov Disord. 2021;36(1):50-58.
15. Bugalho P, Oliveira-Maia AJ. Impulse management issues in Parkinson’s illness: crossroads between neurology, psychiatry and neuroscience. Behav Neurol. 2013;27(4):547-557.
16. Macías-García P, Rashid-López R, Cruz-Gómez ÁJ, et al. Neuropsychiatric signs in clinically outlined Parkinson’s illness: an up to date evaluation of literature. Behav Neurol. 2022;2022:1213393.
17. Cao L, Xu T, Zhao G, et al. Danger components of impulsive-compulsive behaviors in PD sufferers: a meta-analysis. J Neurol. 2022;269(3):1298-1315.
18. Phu AL, Xu Z, Brakoulias V, et al. Impact of impulse management issues on incapacity and high quality of life in Parkinson’s illness sufferers. J Clin Neurosci. 2014;21(1):63-66.
19. Santangelo G, Raimo S, Barone P. The connection between impulse management issues and cognitive dysfunctions in Parkinson’s illness: a meta-analysis. Neurosci Biobehav Rev. 2017;77:129-147.
20. Liu B, Luo W, Mo Y, et al. Meta-analysis of associated components of impulse management issues in sufferers with Parkinson’s illness. Neurosci Lett. 2019;707:134313.
21. Lu HT, Shen QY, Zhao QZ, et al. Affiliation between REM sleep conduct dysfunction and impulsive-compulsive behaviors in Parkinson’s illness: a scientific evaluation and meta-analysis of observational research. J Neurol. 2020;267(2):331-340.
22. Santangelo G, Raimo S, Cropano M, et al. Neural bases of impulse management issues in Parkinson’s illness: a scientific evaluation and an ALE meta-analysis. Neurosci Biobehav Rev. 2019;107:672-685.
23. Weintraub D, Claassen DO. Impulse management and associated issues in Parkinson’s illness. Int Rev Neurobiol. 2017;133:679-717.
24. Weintraub D, Hoops S, Shea JA, et al. Validation of the questionnaire for impulsive-compulsive issues in Parkinson’s illness. Mov Disord. 2009;24(10):1461-1467.
25. Zhang JF, Wang XX, Feng Y, et al. Impulse management issues in Parkinson’s illness: epidemiology, pathogenesis and therapeutic methods. Entrance Psychiatry. 2021;12:635494.
26. Bonfils NA, Benyamina A, Aubin HJ, Luquiens A. Clozapine use for refractory impulse management issues in Parkinson’s illness: a case report. Psychopharmacology (Berl). 2015;232(19):3677-3679.
27. Nardone R, De Blasi P, Höller Y, et al. Repetitive transcranial magnetic stimulation transiently reduces punding in Parkinson’s illness: a preliminary research. J Neural Transm (Vienna). 2014;121(3):267-274.
28. Okai D, Askey-Jones S, Samuel M, et al. Trial of CBT for impulse management behaviors affecting Parkinson sufferers and their caregivers. Neurology. 2013;80(9):792-799.
29. Fang C, Lv L, Mao S, et al. Cognition deficits in Parkinson’s illness: mechanisms and therapy. Parkinsons Dis. 2020;2020:2076942.
30. Guo Y, Xu W, Liu FT, et al. Modifiable threat components for cognitive impairment in Parkinson’s illness: a scientific evaluation and meta-analysis of potential cohort research. Mov Disord. 2019;34(6):876-883.
31. Baiano C, Barone P, Trojano L, Santangelo G. Prevalence and scientific facets of gentle cognitive impairment in Parkinson’s illness: a meta-analysis. Mov Disord. 2020;35(1):45-54.
32. Saredakis D, Collins-Praino LE, Gutteridge DS, et al. Conversion to MCI and dementia in Parkinson’s illness: a scientific evaluation and meta-analysis. Parkinsonism Relat Disord. 2019;65:20-31.
33. Wallace ER, Segerstrom SC, van Horne CG, et al. Meta-analysis of cognition in Parkinson’s illness gentle cognitive impairment and dementia development. Neuropsychol Rev. 2022;32(1):149-160.
34. Severiano E Sousa C, Alarcão J, Pavão Martins I, Ferreira JJ. Frequency of dementia in Parkinson’s illness: a scientific evaluation and meta-analysis. J Neurol Sci. 2022;432:120077.
35. Gibson LL, Weintraub D, Lemmen R, et al. Danger of dementia in Parkinson’s illness: a scientific evaluation and meta-analysis. Mov Disord. 2024;39(10):1697-1709.
36. Xu Y, Yang J, Shang H. Meta-analysis of threat components for Parkinson’s illness dementia. Transl Neurodegener. 2016;5:11.
37. Pang S, Li J, Zhang Y, Chen J. Meta-analysis of the connection between the APOE gene and the onset of Parkinson’s illness dementia. Parkinsons Dis. 2018;2018:9497147.
38. Aarsland D, Batzu L, Halliday GM, et al. Parkinson disease-associated cognitive impairment. Nat Rev Dis Primers. 2021;7(1):47.
39. Skorvanek M, Goldman JG, Jahanshahi M, et al; members of the MDS Score Scales Overview Committee. World scales for cognitive screening in Parkinson’s illness: critique and suggestions. Mov Disord. 2018;33(2):208-218.
40. Hoogland J, van Wanrooij LL, Boel JA, et al; IPMDS Research Group. Detecting gentle cognitive deficits in Parkinson’s illness: comparability of neuropsychological checks. Mov Disord. 2018;33(11):1750-1759.
41. Solar C, Armstrong MJ. Therapy of Parkinson’s illness with cognitive impairment: present approaches and future instructions. Behav Sci (Basel). 2021;11(4):54.
42. Rolinski M, Fox C, Maidment I, McShane R. Cholinesterase inhibitors for dementia with Lewy our bodies, Parkinson’s illness dementia and cognitive impairment in Parkinson’s illness. Cochrane Database Syst Rev. 2012;2012(3):CD006504.
43. Wang HF, Yu JT, Tang SW, et al. Efficacy and security of cholinesterase inhibitors and memantine in cognitive impairment in Parkinson’s illness, Parkinson’s illness dementia, and dementia with Lewy our bodies: systematic evaluation with meta-analysis and trial sequential evaluation. J Neurol Neurosurg Psychiatry. 2015;86(2):135-143.
44. Pagano G, Rengo G, Pasqualetti G, et al. Cholinesterase inhibitors for Parkinson’s illness: a scientific evaluation and meta-analysis. J Neurol Neurosurg Psychiatry. 2015;86(7):767-773.
45. Meng YH, Wang PP, Music YX, Wang JH. Cholinesterase inhibitors and memantine for Parkinson’s illness dementia and Lewy physique dementia: a meta-analysis. Exp Ther Med. 2019;17(3):1611-1624.