Narcolepsy is a power, disabling neurologic dysfunction marked by extreme daytime sleepiness (EDS), disrupted nighttime sleep, cataplexy, sleep paralysis, and hypnagogic hallucinations. As remedy choices develop, clinicians should undertake a complete, customized method to optimize affected person care.
In a current Psychiatric Instances Case-Based mostly Psych Views program titled “Optimizing Narcolepsy Administration in Grownup Sufferers,” Nishi Bhopal, MD, a psychiatrist and founding father of Pacific Integrative Psychiatry in San Francisco, California; and Ellen Wermter, FNP, a board-certified household nurse practitioner at Restorative Sleep Medication in Charlottesville, Virginia, offered scientific circumstances and remedy methods with an emphasis on collaborative care. Their dialogue gives vital steering for psychological well being professionals, who are sometimes the primary level of contact for undiagnosed or misdiagnosed sufferers.
Diagnostic Panorama and Challenges
Narcolepsy is underdiagnosed, with a median delay to prognosis exceeding 10 years. This delay stems from restricted entry to sleep specialists, overlapping psychiatric displays (significantly despair), and low public and clinician consciousness. Correct prognosis depends on scientific historical past, polysomnography, and the a number of sleep latency take a look at, together with cerebrospinal fluid hypocretin ranges in sure circumstances.
Psychological well being clinicians should preserve excessive suspicion when treating sufferers with persistent fatigue, poor focus, and temper issues that don’t reply to plain psychiatric interventions. It’s vital to acknowledge the total syndrome of narcolepsy signs to information acceptable sleep testing and referral.
Case-Based mostly Method to Customized Remedy
Two scientific circumstances highlighted the significance of individualized administration.
Case 1: A 32-year-old man with EDS and cataplexy (4-5 episodes per week) met standards for narcolepsy sort 1. His remedy preferences included avoiding stimulants or managed substances as a consequence of a household historical past of substance use. Laboratory research confirmed low hypocretin ranges and goal indicators of fast eye motion (REM) intrusions.
Case 2: A 26-year-old lady with narcolepsy sort 2 (EDS, sleep paralysis, and hallucinations with out cataplexy) reported inadequate aid with modafinil and requested improved alertness and day by day perform. Her case was sophisticated by iron deficiency anemia (ferritin = 26 ng/mL) and migraine.
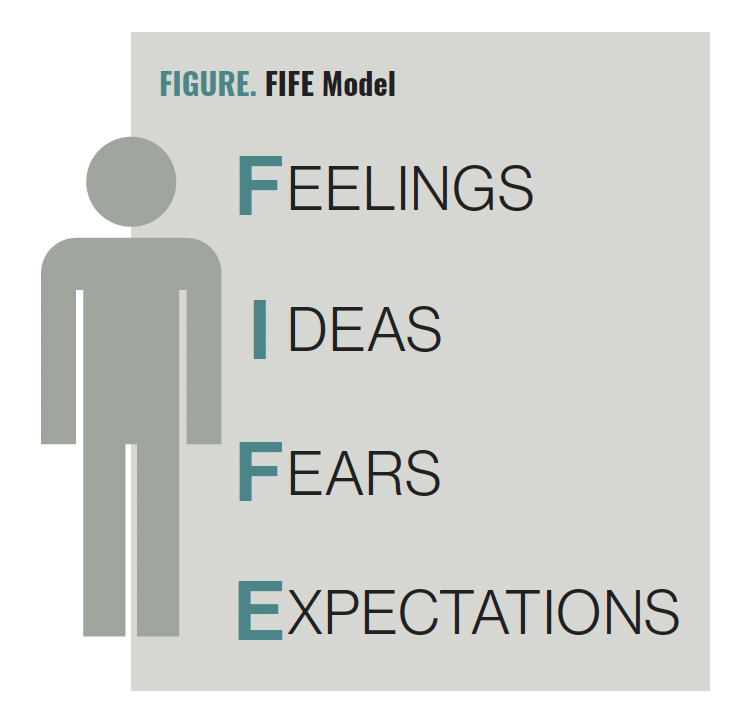
In each circumstances, the clinicians emphasised the worth of shared decision-making and aligning remedy with affected person values, preferences, and comorbidities. The usage of structured frameworks such because the FIFE mannequin (emotions, concepts, functioning, expectations; Determine) was really useful to elicit affected person targets.
Treatment Overview and Concerns
The remedy panorama has expanded considerably prior to now 5 years, providing a number of choices throughout a number of pharmacologic lessons:
- Pitolisant (Wakix): A histamine-3 receptor inverse agonist, authorised for EDS and cataplexy. Notably, it’s a nonscheduled treatment, making it significantly appropriate for sufferers involved about managed substances. Pitolisant requires QTc monitoring as a consequence of cardiac dangers and takes time to titrate.
- Solriamfetol (Sunosi): A dopamine/norepinephrine reuptake inhibitor authorised for EDS, providing prolonged wakefulness (as much as 9 hours) with a comparatively easy pharmacodynamic profile. It lacks important hormonal contraception interplay, a bonus for sufferers of reproductive age.
- Oxybate therapies (eg, low-sodium oxybate/Xywav): Present advantages throughout the symptom spectrum, resembling EDS, cataplexy, and fragmented sleep. These drugs act by way of γ-aminobutyric acid modulation and are delivered by way of a Threat Analysis and Mitigation Technique program as a consequence of security and abuse potential. Clinicians should information sufferers by way of onboarding, security monitoring, and antagonistic impact administration.
Many sufferers require multimodal remedy, combining brokers focusing on distinct neurotransmitter methods. For instance, combining pitolisant for daytime signs and oxybate remedy at night time could enhance each REM stability and application.
“After I first began in sleep medication about 8 years in the past, there have been just a few drugs that have been FDA authorised for the remedy of narcolepsy. However within the final 5 years, now we have seen an addition of a number of new drugs,” stated Wermter. “Now there are a lot of extra selections for sufferers with narcolepsy to have the ability to discover the remedy that they want. It’s great to see how the panorama is bettering as a result of now we have so many instruments accessible to us.”
Behavioral and Life-style Interventions
Pharmacologic remedy alone is inadequate. Nonpharmacologic methods, typically overseen by psychiatrists and therapists, are important to stabilizing circadian rhythms and decreasing symptom burden:
- Scheduled naps: Strategically positioned 15- to 30-minute naps enhance daytime functioning. Some sufferers are nonresponders; clinicians should personalize nap size and timing.
- Dietary counseling: Given the elevated metabolic threat in narcolepsy, whole-food diets with low glycemic variability are most well-liked. Rising proof suggests ketogenic diets could also be useful, mirroring approaches in epilepsy.
- Mild remedy and sleep hygiene: Vivid morning gentle, constant wake occasions, and decreased night stimulation are central to circadian stabilization.
- Cognitive behavioral remedy for hypersomnia: A promising structured intervention, now accessible by way of specialised applications, gives psychosocial help for sufferers typically stigmatized or misunderstood.
Psychiatrists are significantly positioned to help the emotional toll of dwelling with narcolepsy and to determine comorbid situations—most notably despair and anxiousness, which happen at larger charges on this inhabitants.
Monitoring, Adherence, and Lengthy-Time period Care
Monitoring response to remedy consists of common evaluation utilizing instruments just like the Epworth Sleepiness Scale however ought to prolong to qualitative experiences of alertness, focus, and emotional well-being. Sufferers could expertise decreased efficacy as a consequence of exterior stressors, sleep schedule disruptions, or evolving life calls for.
Adherence challenges embrace the next:
- Forgetfulness and sleep inertia (alleviated by behavior stacking, pillboxes, and alarms)
- Value and entry points, particularly throughout insurance coverage transitions
- Psychosocial issues (stigma, need to really feel “regular,” treatment fatigue)
Psychological well being clinicians can help adherence by way of behavioral teaching, motivational interviewing, and fascinating caregivers. Importantly, sufferers must be reminded that narcolepsy is a lifelong neurologic dysfunction, requiring long-term help and medicine.
Office and Incapacity Concerns
Office lodging below the People with Disabilities Act must be mentioned. Versatile begin occasions, scheduled breaks, distant work choices, and guarded nap occasions can considerably enhance perform and job retention.
Clinicians could help with incapacity documentation, testing lodging, and academic helps for college kids with narcolepsy.